HPV twist?
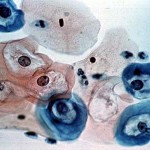 Human Papilloma Virus (HPV) is a family of small, non-enveloped DNA viruses which infect epithelial cells, and of which there are over 100 subtypes. HPV is divided into two major categories, high risk types which includes types 16, 18, 31. 33, 35. 39, 45, and low risk types 6 and 11. HPV 16 is implicated in over 90% of cervical cancers and shown to be a causal factor in the development of the disease. HPV produces two oncoproteins, E6 and E7, which inactivate the cellular tumor suppressor proteins, p53 and pRB respectively. This allows it to disable two of the cell’s major tumor suppressor mechanisms.
Human Papilloma Virus (HPV) is a family of small, non-enveloped DNA viruses which infect epithelial cells, and of which there are over 100 subtypes. HPV is divided into two major categories, high risk types which includes types 16, 18, 31. 33, 35. 39, 45, and low risk types 6 and 11. HPV 16 is implicated in over 90% of cervical cancers and shown to be a causal factor in the development of the disease. HPV produces two oncoproteins, E6 and E7, which inactivate the cellular tumor suppressor proteins, p53 and pRB respectively. This allows it to disable two of the cell’s major tumor suppressor mechanisms.
HPV is not only limited to cervical cancer, but has also been implicated in squamous cell carcinomas of the head and neck regions (HNSCC) and includes oral, tonsillar, and oropharyngeal tumors—which have usually been associated with long term alcohol and tobacco usage. The incidence of HNSCC has risen steadily over the last 20-30 years in younger patients, and about 20% of these carcinomas are HPV positive with HPV type 16 emerging as the most prevalent subtype present in these tumors.
However, unlike the clinical regimen for cervical carcinoma which includes HPV typing of the tumor tissue, there are currently no standard molecular tests utilized as part of the clinical treatment protocols for head and neck cancers. Prognostic factors for survival include molecular diagnostic testing for cytokines, proteomic profiling, and testing for the presence of HPV.
Interestingly, the detection of HPV in head and neck cancer is a favorable prognostic marker; HPV positive tumors are biologically distinct from HPV negative tumors which are typically associated with long-term tobacco and alcohol use. This favorable prognostic factor in younger patients with HPV positive tumors may be attributed to the lack of p53 mutations found in younger patients, and thus improves chemotherapeutic treatment response in these patients, in part because the efficacy of chemotherapy depends upon a functional p53 gene that mediates apoptosis (programmed cell death) in response to radiation and chemotherapy.
Note: the thumbnail above shows visibly HPV-infected cells
| Print article | This entry was posted by rios on November 17, 2009 at 1:21 pm, and is filed under Inside Cancer. Follow any responses to this post through RSS 2.0. You can skip to the end and leave a response. Pinging is currently not allowed. |